Hypertension, also known as high blood pressure, is a common medical condition that affects millions of people worldwide. It occurs when the force of the blood pushing against the artery walls is consistently high, causing the heart to work harder to pump blood. Hypertension is defined as having a systolic blood pressure (the top number) of 140 mmHg or higher, and/or a diastolic blood pressure (the bottom number) of 90 mmHg or higher. Often referred to as the "silent killer," hypertension often doesn't show symptoms, but if left uncontrolled, it can lead to serious health problems such as heart attacks, strokes, or organ failure by damaging blood vessels, the heart, kidneys, and other organs.
Hypertension has become a global health concern, with approximately one in three adults worldwide affected by it[1]. According to the World Health Organization (WHO), an estimated 1.13 billion people worldwide have hypertension, contributing to around 7.5 million deaths each year. However, many individuals with hypertension are either unaware of their condition or do not have it properly managed. It is essential to raise awareness and improve the prevention and management of hypertension to reduce its burden and associated complications.
Unhealthy lifestyle choices, such as consuming a high-sodium diet, being sedentary, excessive alcohol intake, and smoking, significantly increase the risk of developing hypertension. Additionally, obesity and underlying health conditions like chronic kidney disease, diabetes, and certain hormonal disorders are also associated with hypertension. Prevention involves effectively managing and controlling these risk factors through lifestyle modifications. This includes adopting a healthy diet, engaging in regular physical activity, managing stress, reducing salt intake, limiting alcohol consumption, and quitting smoking. In some cases, medication may be necessary to effectively manage blood pressure levels. Commonly prescribed hypertension medications include ACE inhibitors, angiotensin-2 receptor blockers (ARBs), calcium channel blockers, diuretics, and beta blockers. The ultimate goal is to reduce overall risks for complications and mortality associated with hypertension.
Animal models play a significant role in understanding the mechanisms of hypertension, developing new treatments, and exploring potential therapeutic interventions. Currently, commonly used animal models include[2,3]:
1. Spontaneously Hypertensive Rat (SHR) Model: The SHR model closely resembles human hypertension and does not require special diets during breeding. These rats develop hypertension with blood pressure starting to rise at 4-6 weeks of age, exceeding 160mmHg by 16 weeks of age. The advantages of this model include a high incidence of hypertension and cardiovascular diseases, a relatively short disease course, and the ability to observe pathological changes in target organs affected during disease progression. However, breeding SHR rats has specific requirements and a relatively long breeding cycle. Additionally, there are challenges associated with genetic breeding, such as genetic variation, strain discontinuity, and difficulties in large-scale usage.
2. Renovascular Hypertension Models: These models involve constricting one or both renal arteries, reducing renal blood flow and activating the renin-angiotensin system. This leads to increased production of angiotensin II, a potent vasoconstrictor, and stimulator of aldosterone secretion.
3. Genetically Modified Mouse Models: These models, such as AGT-REN transgenic hypertensive mice, are created through genetic engineering techniques, enabling researchers to introduce specific gene mutations related to hypertension. They can help elucidate the genetic factors involved in the development and progression of hypertension.
4. Neurogenic Hypertension Models: These models involve stimulating or inhibiting neural pathways that control blood pressure, such as the sympathetic nervous system, the baroreflex, and the central nervous system.
5. Endocrine Hypertension Models: These models involve administering or depriving hormones that influence blood pressure, such as aldosterone, cortisol, thyroid hormones, and sex hormones.
Each animal model for studying hypertension has its advantages and limitations. It is important to choose an appropriate model that aligns with the research question and validate the findings in humans.
Angiotensinogen (AGT) serves as a substrate for renin (REN) and acts as a precursor for all angiotensin peptides. Research indicates that excessive activation of the renin-angiotensin system (RAS) is the primary cause of hypertension. REN hydrolyzes AGT, producing angiotensin I (Ang I), which is then converted into the potent vasoconstrictor angiotensin II (Ang II) through the action of angiotensin-converting enzyme (ACE). Ang II exerts a potent vasoconstrictive effect, leading to elevated blood pressure and the onset of hypertension[4]. Furthermore, studies have reported the direct involvement of AGT in blood pressure regulation. Perivascular adipose tissue (PVAT), a layer of adipose tissue surrounding blood vessels, expresses high levels of AGT. Inhibiting AGT expression in PVAT can lower blood pressure levels, revealing the significant role of AGT in the development of hypertension[5].
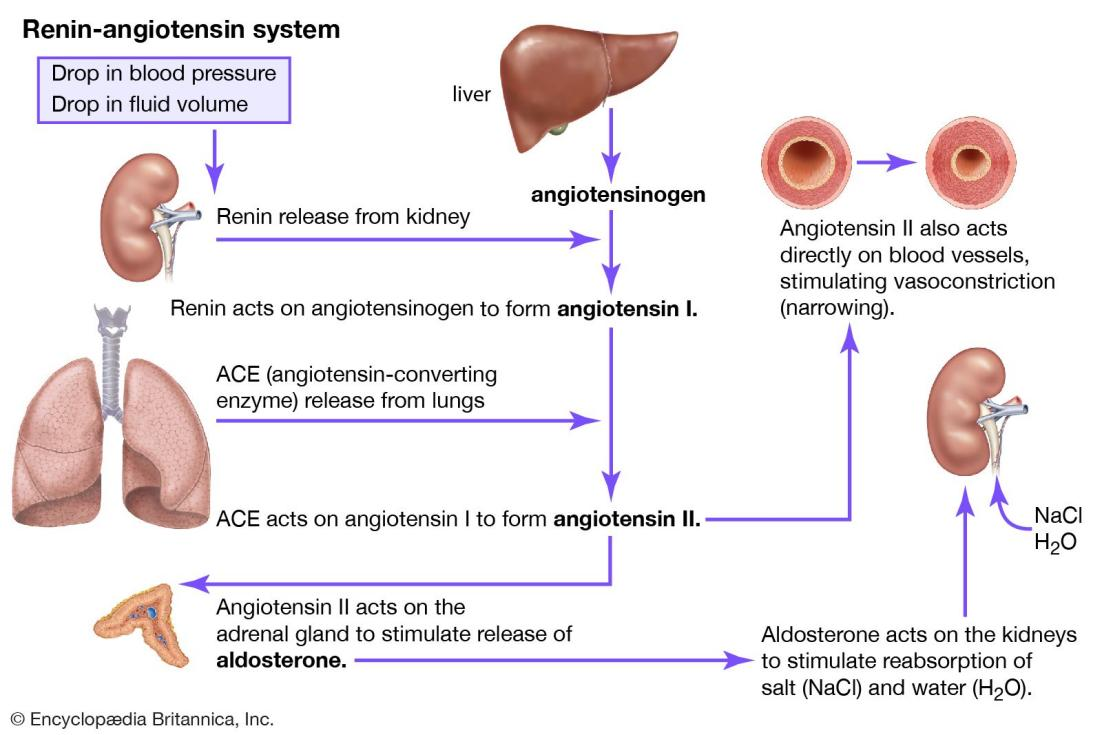
Renin-angiotensin system[6]
At GemPharmatech, we have utilized gene editing technology to replace the coding region and 3' UTR region of the Agt gene in C57BL/6JGpt mice with the corresponding human sequences, resulting in the generation of a fully humanized AGT mouse model (B6-hAGT, No. T054372). This model expresses human AGT and can be used for studying hypertension-related mechanisms, evaluating the efficacy of AGT-targeting antihypertensive drugs, and conducting drug screening. We also offer products and services for hypertension models induced by Ang II, L-NAME, or DOCA. Additionally, we are actively developing a double-gene humanized mouse model (B6-H11-hREN / B6-hAGT) that can simultaneously express human AGT and REN. Theoretically, this humanized mouse model can spontaneously develop hypertension, meeting the research needs for evaluating antihypertensive drug efficacy. Contact us to explore what we can do for you.
Reference:
1. https://www.who.int/news-room/fact-sheets/detail/hypertension
2. Lerman LO, Kurtz TW, Touyz RM, Ellison DH, Chade AR, Crowley SD, Mattson DL, Mullins JJ, Osborn J, Eirin A, Reckelhoff JF, Iadecola C, Coffman TM. Animal Models of Hypertension: A Scientific Statement From the American Heart Association. Hypertension. 2019 Jun;73(6):e87-e120.
3. Lerman LO, Chade AR, Sica V, Napoli C. Animal models of hypertension: an overview. J Lab Clin Med. 2005 Sep;146(3):160-73.
4. Lu, H., Cassis, L. A., Kooi, C. W., & Daugherty, A. (2016). Structure and functions of angiotensinogen. Hypertension Research, 39, 492–500.
5. Xu Y, Rong J, Zhang Z. The emerging role of angiotensinogen in cardiovascular diseases. J Cell Physiol. 2021;236(1):68-78.
6. Britannica, The Editors of Encyclopaedia. "renin-angiotensin system". Encyclopedia Britannica, 11 Feb. 2023, https://www.britannica.com/science/renin-angiotensin-system. Accessed 23 May 2023.


